The gut microbiome, an intricate community of microorganisms residing in our digestive tract, plays a pivotal role in shaping our health and disease states. Recent research has illuminated its significant influence on the immune system, particularly in the context of autoimmune diseases. This article delves into the complex relationship between the gut microbiome and the development of autoimmune conditions, exploring the mechanisms at play and the potential for therapeutic interventions.
Autoimmune diseases arise when the immune system mistakenly attacks the body’s own cells, leading to chronic inflammation and tissue damage. Examples include rheumatoid arthritis, multiple sclerosis, and type 1 diabetes. The causes of these diseases are multifactorial, involving genetic susceptibility, environmental triggers, and immune system dysregulation. Increasingly, the gut microbiome is recognized as a critical player in this intricate dance.
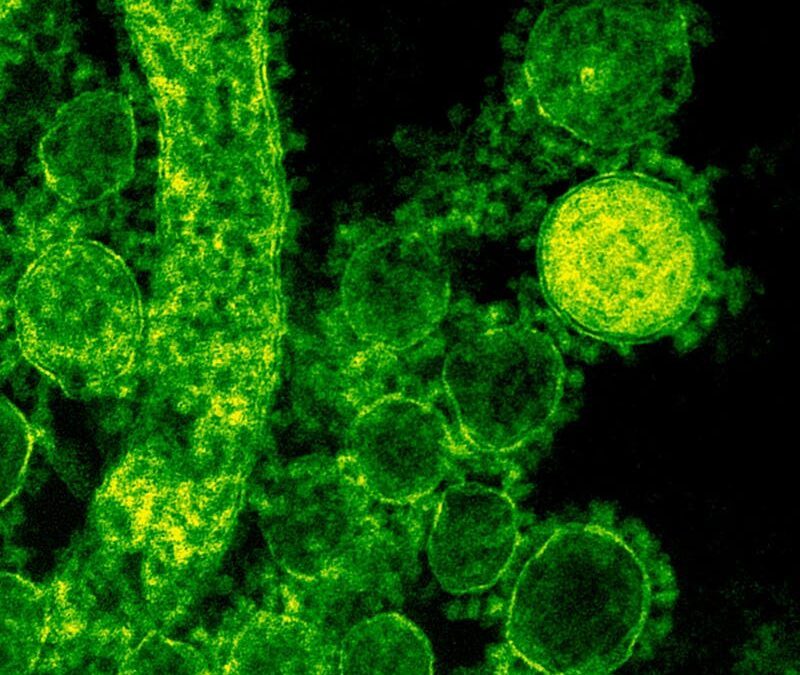
The gut microbiome consists of trillions of bacteria, viruses, fungi, and other microorganisms that inhabit our gastrointestinal tract. These microbes are not merely passive inhabitants; they engage in a dynamic interplay with our immune system. They help in digesting food, producing vitamins, and warding off harmful pathogens. Beyond these functions, they are pivotal in educating and regulating the immune system, thus influencing its response to various stimuli.
Research has shown that alterations in the composition and function of the gut microbiome, known as dysbiosis, can predispose individuals to autoimmune diseases. Dysbiosis can lead to a breach in the intestinal barrier, often referred to as “leaky gut,” allowing microbes and microbial products to enter the bloodstream. This breach can trigger an abnormal immune response, which, in genetically susceptible individuals, may escalate into an autoimmune condition.
Several mechanisms have been proposed to explain how the gut microbiome influences autoimmune disease development. These include molecular mimicry, where microbial antigens resemble self-antigens, leading the immune system to attack both; and the alteration of regulatory T cell function, which is crucial for maintaining immune tolerance to self-antigens.
The gut microbiome’s influence on autoimmune diseases is also evident in the role of diet and antibiotics, which can significantly affect microbial composition. Diets high in fiber, for instance, have been associated with a diverse and stable microbiome, which may confer protection against autoimmune diseases. Conversely, antibiotic use, particularly in early life, has been linked to disruptions in the microbial community and an increased risk of autoimmune conditions.
Given the gut microbiome’s role in autoimmune diseases, it presents a promising target for therapeutic intervention. Probiotics, prebiotics, and fecal microbiota transplantation are being explored as potential treatments to restore a healthy microbiome balance. Personalized nutrition, targeting specific microbial profiles, also holds promise in preventing or alleviating autoimmune responses.
In conclusion, the gut microbiome plays a crucial role in the development and progression of autoimmune diseases. Its interaction with our immune system is complex and multifaceted, influencing disease susceptibility and offering new avenues for prevention and treatment. Further research is needed to fully understand these relationships and to harness the microbiome’s potential in combating autoimmune diseases effectively.