Recent studies have hinted at the intriguing possibility that certain drugs used in the treatment of rheumatic diseases might also have beneficial effects in preventing or delaying the development of Alzheimer’s disease. This article delves into the emerging research surrounding the repurposing of rheumatic drugs for Alzheimer’s, exploring the mechanisms through which these medications could exert their protective effects, and examining the implications for future treatment strategies.
Rheumatic diseases are a diverse group of disorders characterized by inflammation and pain in the musculoskeletal system. Some of the most commonly prescribed medications for these conditions include Arava, Enbrel, Rinvoq, Humira, Xeljanz, Skyrizi, Tremfya, Remicade, Cimzia, Simponi, Simponi Aria, Orencia, Cosentyx, Taltz, Otezla, Hevzara, and Actemra. These drugs work through various mechanisms to reduce inflammation and modulate the immune system’s activity.
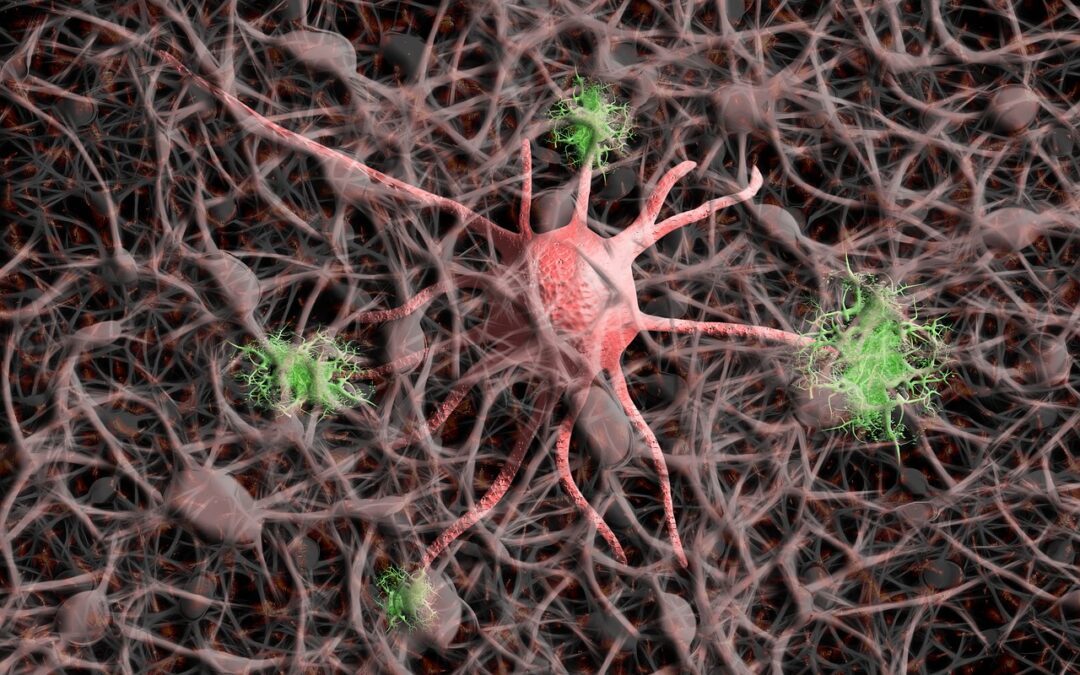
Alzheimer’s disease, on the other hand, is a progressive neurodegenerative disorder marked by the accumulation of amyloid-beta plaques and tau tangles in the brain, leading to cognitive decline and memory loss. While the primary risk factors for Alzheimer’s include age, genetics, and lifestyle, increasing evidence suggests that inflammation plays a significant role in the disease’s pathogenesis.
The connection between rheumatic drugs and Alzheimer’s lies in the inflammatory processes common to both conditions. Several of these medications have been found to lower the levels of pro-inflammatory cytokines, which are elevated in both rheumatic diseases and Alzheimer’s. By reducing systemic inflammation, these drugs could potentially slow down or prevent the neuroinflammatory processes that contribute to Alzheimer’s pathology.
Research into the repurposing of rheumatic drugs for Alzheimer’s is still in its early stages, but preliminary studies and clinical trials have shown promising results. For instance, TNF inhibitors, such as Enbrel and Humira, have been observed to mitigate cognitive decline in some Alzheimer’s patients. Similarly, drugs targeting interleukin-1 and interleukin-6, like Anakinra (not listed previously but similar in function to some drugs mentioned), have also shown potential in reducing neuroinflammation and improving cognitive functions in preclinical models.
These findings open up new avenues for Alzheimer’s research and treatment. The repurposing of existing rheumatic drugs could offer a faster, more cost-effective path to developing new therapies for Alzheimer’s, given that these medications have already been approved for other conditions and their safety profiles are well-documented. However, it is crucial to conduct more extensive clinical trials to understand the efficacy, optimal dosages, and potential side effects of these drugs when used to treat Alzheimer’s.
In conclusion, the possible beneficial effects of rheumatic drugs on developing Alzheimer’s highlight an exciting frontier in the fight against this debilitating disease. While further research is needed to fully understand the mechanisms and impact of these drugs on Alzheimer’s, the potential to repurpose existing medications offers hope for more effective treatment options in the near future.