This study focused on comparing the frequency of serositis, which refers to inflammation of the lining around the heart (pericarditis) and lungs (pleuritis), between patients with rheumatoid arthritis (RA) and psoriatic arthritis (PsA). These conditions are types of autoimmune diseases that can cause inflammation in various parts of the body, but there has been limited research on how often PsA patients experience serositis, compared to RA patients, who are known to have a significant risk.
Study Purpose:
The primary goal was to estimate how often pleuropericarditis (a combined term for pericarditis and pleuritis) occurs in PsA patients compared to RA patients. While it is known that between 30% and 50% of RA patients can develop pericarditis, the frequency in PsA has not been well-defined. This study aimed to fill that gap by comparing the two groups of patients and their rates of serositis.
Methods:
The researchers conducted a retrospective chart review, meaning they looked back at patient records from 2013 to 2021, focusing on people who were hospitalized during this time. A total of 113 inpatients, between the ages of 18 and 65, were included in the study:
• Group 1: 57 patients with rheumatoid arthritis (RA)
• Group 2: 56 patients with psoriatic arthritis (PsA)
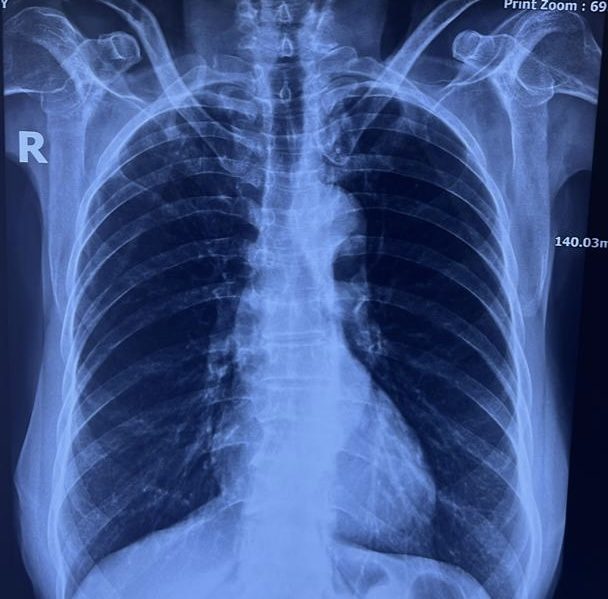
The researchers specifically looked for instances of pericardial or pleural effusions, which are abnormal buildups of fluid in the linings of the heart and lungs. These fluid buildups can be signs of pericarditis or pleuritis, respectively.
Results:
The study found that:
• In RA patients (Group 1): Out of the 57 patients, 48 had pericardial or pleural effusions. Of these 48 cases, 46 (81%) were labeled as idiopathic, meaning there was no identifiable cause for the fluid buildup.
• In PsA patients (Group 2): Out of the 56 patients, 42 had pericardial or pleural effusions. However, only 23 of these cases (41%) were considered idiopathic.
This difference was statistically significant (P < 0.0001), showing that RA patients are much more likely to have idiopathic pericardial or pleural effusions compared to PsA patients.
Conclusion:
The findings suggest that while both RA and PsA can cause pleuropericarditis (inflammation of the heart and lung linings), RA patients are much more likely to develop these conditions without a clear cause (idiopathic). In fact, RA patients were found to be about twice as likely to have idiopathic pericardial or pleural effusions compared to PsA patients.
Implications:
This study highlights that serositis is a concern for both RA and PsA patients, but RA patients may be at higher risk for developing these conditions without a known reason. The researchers recommend that further studies with larger patient groups be conducted to better understand the frequency of serositis, especially in PsA patients, where data is still limited.
This research adds to the understanding of how autoimmune diseases like RA and PsA can affect the heart and lungs, helping doctors better assess and manage the risk of serositis in these patients.